Hyperalgesia is a condition where a person develops an increased sensitivity to pain. What may not hurt most people can cause significant pain in an individual with hyperalgesia. Although there are many potential causes associated with hyperalgesia, the condition is thought to be the result of changes to nerve pathways, which cause a person's nerves to have an overactive response to pain. Medications are available to prevent a person's symptoms from worsening.
Source
Causes
There are several nerve or "pain" pathways in the body where signals can start to miscommunicate with each other, resulting in hyperalgesia. Some scientists think that hyperalgesia occurs when chemicals known to reduce pain are disrupted; others propose that hyperalgesia happens when "crossed wires" in the nervous system prevent pain signals from transmitting accurately.
Types
Doctors usually divide hyperalgesia into primary and secondary categories. Both of these conditions are due to initial tissue trauma and inflammation.
Primary hyperalgesia
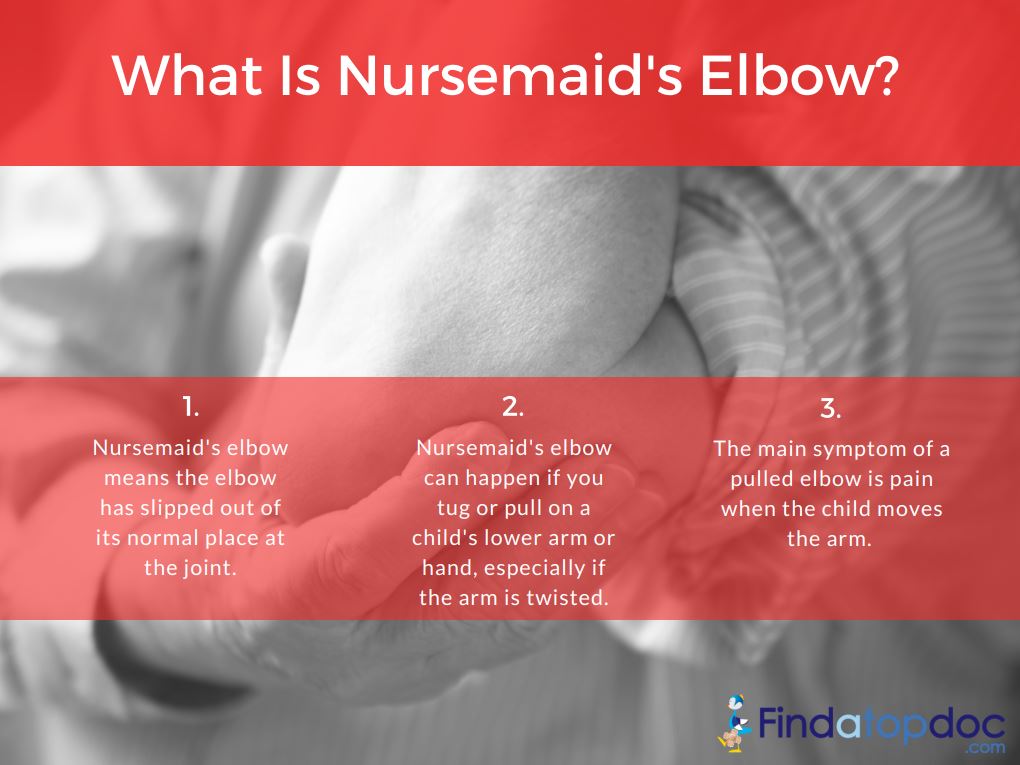
This type of hyperalgesia is when the increased pain occurs in the tissue where the injury took place. An example would be when a person has surgery on their elbow, and the pain starts to worsen over time instead of improving.
Secondary hyperalgesia
This type occurs when the pain seems to spread to non-injured tissue or tissues.
Another kind of hyperalgesia is opioid-induced hyperalgesia (OIH). OIH occurs when a person experiences worsening or new pain as a result of taking opioids, such as morphine, hydrocodone, or fentanyl for pain relief.
Treatment
If hyperalgesia is opioid induced, a doctor may reduce the dosage. While a person may experience an initial increase in pain due to these changes, this frequently gives way to a reduced pain experience in those with hyperalgesia. A doctor may also try to prescribe an alternative, non-opioid medication.
There are also different classes of opioids a doctor could prescribe. One example is methadone, a medication that relieves pain, yet has been shown to prevent or reduce OIH. However, it is still possible that a person could have hyperalgesia while taking methadone. Another medication is buprenorphine, which can help to reduce the incidence of hyperalgesia by blocking receptors in the brain and spinal cord.
Ketamine, which also blocks certain receptors, is another option. All of these medications, as well as methadone, require close medical supervision. Another option is a muscle or nerve block, which uses a local anesthetic to numb or delay painful nerve impulses. Sometimes, treating hyperalgesia requires a trial-and-error approach, with frequent adjustments to medication until a person achieves a reduced pain experience.
Symptoms
The chief symptom of hyperalgesia is an increasingly extreme reaction to painful stimuli without any new injuries or worsening of a medical condition. An example would be a surgical incision that becomes more painful over time, yet the wound is not infected, and a person has not experienced any further injury.Hyperalgesia is different from tolerance to medications although the two processes are similar.
If a person develops a tolerance to a particular drug, it usually means that their body has become accustomed to the presence of the drug at the current dosage, and the drug is no longer working properly. When a person has developed a tolerance to a drug, increasing the dosage will usually decrease a person's pain.
Drug tolerance is different from hyperalgesia, where increasing pain medication will not reduce the amount of pain a person feels. Sometimes, increasing the pain medication makes the person's pain worse.
Another similar medical condition is allodynia. This condition is where a person develops a significant pain response to non-painful stimuli. Even brushing against a person's skin can cause pain.In hyperalgesia, a person has experienced a painful stimulus, such as cancer pain or pain following surgery, but their response to the pain is greater than the expected level of pain.
A doctor may increase a person's pain medication to determine if hyperalgesia is the cause. If the additional pain medication does cause more pain, it is possible the condition is hyperalgesia. Currently, there are no definitive diagnostic tests for hyperalgesia.